Festoons
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
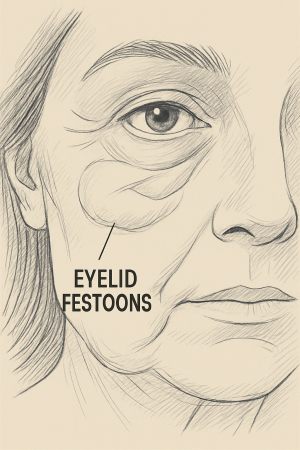
Festoons, also known as malar mounds, represent a complex cosmetic and functional challenge, characterized by the formation of redundant, sagging tissue along the lower eyelid and upper cheek. These formations are often attributed to a combination of factors, including fluid accumulation, soft tissue laxity, and underlying structural changes in the periorbital region[1]. Differentiating festoons from other conditions affecting the lower eyelid and cheek, such as malar edema and simple skin laxity, is crucial for appropriate management[2]. The intricate anatomy of the periorbital region, encompassing the skin, subcutaneous fat, muscle, and underlying bony structures, contributes to the varied presentation and treatment approaches for festoons[2]. The impact of festoons extends beyond mere cosmetic concerns, potentially affecting vision and causing significant psychological distress for affected individuals[3]. A comprehensive understanding of the etiology, pathophysiology, and available treatment modalities is essential for clinicians to effectively address this condition and improve patient outcomes[4].
General Overview
Signs of aging in the lower eyelid region, such as festoons, are a common issue that can impact an individual's appearance and quality of life. The exact prevalence of festoons is difficult to determine due to variations in diagnostic criteria and the fact that many individuals may not seek medical attention for cosmetic concerns. Festoons are characterized by a distinct bulging or swelling of the skin and soft tissues in the malar region, which is located between the lower eyelid and the cheek. This condition is often associated with aging, sun exposure, and genetic predisposition, but can also arise secondary to other underlying medical conditions. The manifestations of festoons can range from mild prominence to significant disfigurement, causing patients to seek both surgical and non-surgical interventions to improve their appearance.
Disease Entity
Malar mounds, or festoons, are chronic collections of edematous soft tissue localized to the infraorbital and malar regions. They are considered a distinct entity within the spectrum of lower eyelid and midface aging changes, distinguishable from other conditions such as malar edema, which involves transient fluid accumulation, and age-related skin laxity, which lacks the distinct mound-like appearance. The pathophysiology involves a complex interplay of factors, including weakening of the orbital septum, herniation of orbital fat, and alterations in the lymphatic drainage of the lower eyelid and cheek. The condition is often progressive, with the severity increasing over time due to continued collagen breakdown and loss of skin elasticity. Diagnosis of festoons typically relies on clinical examination, with careful assessment of the location, size, and consistency of the swelling, as well as evaluation for any associated signs of inflammation or underlying pathology. Given the significant impact on appearance and the potential for functional impairment, understanding the disease entity of festoons is critical for clinicians to provide appropriate and effective management strategies.
Disease
In addition to being a cosmetic concern, festoons are a manifestation of underlying structural and functional changes within the periorbital tissues. These changes can lead to a cascade of effects, including impaired lymphatic drainage, increased fluid retention, and progressive weakening of the supporting structures of the lower eyelid and cheek. The disease process involves a complex interplay of factors, including genetic predisposition, environmental influences, and age-related tissue degeneration. The symptoms of festoons can range from mild puffiness and swelling to significant disfigurement, with the potential to cause visual impairment and psychological distress. Accurate diagnosis and appropriate management are essential to address the underlying disease process and improve patient outcomes.
Etiology and Risk Factors
The etiology of festoons is multifactorial, encompassing genetic predisposition, environmental influences, and intrinsic aging processes. Genetic factors play a significant role, with some individuals exhibiting a higher propensity for developing festoons due to inherited traits [5]. Prolonged exposure to ultraviolet radiation from the sun is a well-established risk factor, as it accelerates collagen breakdown and elastin damage, leading to premature skin aging and increased laxity[6]. Smoking is another significant environmental factor that contributes to festoon development. Studies have shown how smoking affects the skin, particularly in terms of facial aging [7]. Age-related changes, such as the weakening of the orbital septum and the descent of the malar fat pad, contribute to the formation of festoons by creating a space for fluid accumulation and soft tissue sagging. Moreover, certain medical conditions, such as thyroid disorders and renal dysfunction, can exacerbate fluid retention and contribute to the development or worsening of festoons. Previous trauma or surgery to the periorbital region can also disrupt lymphatic drainage and contribute to the formation of festoons. Understanding these diverse etiological factors and risk factors is crucial for clinicians to develop personalized prevention and treatment strategies for patients with festoons.
General Pathology
The general pathology of festoons involves a complex interplay of histological and structural changes within the skin, subcutaneous tissues, and underlying musculature of the lower eyelid and cheek. Histologically, festoons exhibit a characteristic pattern of collagen and elastin fiber degradation, with a reduction in the density and organization of these structural proteins. High-frequency ultrasounds have shown that these skin parameters change with age[8]. This leads to a loss of skin elasticity and resilience, contributing to the sagging and bulging appearance of festoons. There is also a decrease in the number of fibroblasts, which are responsible for synthesizing collagen and elastin, further compromising the structural integrity of the skin[9]. Additionally, festoons often exhibit an accumulation of fluid within the interstitial spaces of the dermis and subcutaneous tissues, contributing to the swelling and "puffy" characteristic of the condition. Changes in the extracellular matrix are also evident, with alterations in the composition and distribution of glycosaminoglycans, such as hyaluronic acid, which play a crucial role in maintaining skin hydration and elasticity[10].
Pathophysiology
The pathophysiology of festoons is complex, involving a combination of factors that contribute to the characteristic swelling and sagging of the lower eyelids and cheeks. While not specific to festoons, alterations in lymphatic outflow have been implicated in the pathophysiology of edema in various contexts[11]. Disruption of normal lymphatic drainage can contribute to fluid accumulation and tissue swelling, which may play a role in the development or exacerbation of lower eyelid contour abnormalities. One key element is the weakening of the orbital septum, which normally acts as a barrier to prevent the protrusion of orbital fat. As the orbital septum weakens with age, orbital fat can herniate forward, contributing to the bulge associated with festoons. The location, size, and consistency of the swelling, as well as evaluation for any associated signs of inflammation or underlying pathology should be carefully assessed [12]. Furthermore, age-related changes in the malar fat pad, a prominent fat compartment in the cheek, can contribute to the development of festoons. With aging, the malar fat pad descends and loses volume, leading to a loss of support for the overlying skin and soft tissues, resulting in sagging and the formation of festoons[13]. Moreover, the accumulation of fluid within the subcutaneous tissues plays a significant role in the pathophysiology of festoons. Impaired lymphatic drainage and increased vascular permeability can lead to fluid retention, exacerbating the swelling and puffiness associated with the condition[14]
Primary Prevention
Primary prevention of festoons involves adopting lifestyle modifications and skincare practices that minimize risk factors and promote skin health.
Minimizing sun exposure: protecting the skin from excessive sun exposure is paramount. This includes regular use of broad-spectrum sunscreens with a high sun protection factor, wearing protective clothing such as hats and sunglasses, and avoiding prolonged sun exposure during peak hours.
Smoking cessation: smoking accelerates collagen breakdown and impairs skin elasticity.
Healthy Diet: maintaining a healthy diet rich in antioxidants, vitamins, and minerals can further protect the skin from damage and promote collagen production[15]. Proper hydration is essential for maintaining skin elasticity and reducing the appearance of fine lines and wrinkles[16].
Diagnosis
The diagnosis of festoons typically relies on a comprehensive clinical evaluation, including a thorough history and physical examination. The patient's history should include inquiries about:
The onset and duration of the swelling
Any associated symptoms such as itching or pain
Any potential contributing factors such as sun exposure, smoking, or underlying medical conditions.
The clinician should carefully examine the periorbital region, noting the size, shape, and location of the swelling, as well as any associated skin changes such as discoloration, texture irregularities, or telangiectasias.
Palpation of the affected area can help assess the consistency of the swelling and identify any underlying masses or nodules. In some cases, imaging studies such as magnetic resonance imaging or computed tomography may be necessary to rule out other potential causes of facial swelling.
History
In taking the history of a patient presenting with festoons, it is crucial to gather detailed information about the evolution, duration, and potential exacerbating factors of the condition. Eliciting a comprehensive medical history, including any underlying medical conditions such as thyroid disorders, renal dysfunction, or cardiovascular disease, is essential, as these conditions can contribute to fluid retention and exacerbate festoons. Inquiring about prior facial surgeries or cosmetic procedures is also important, as such interventions may disrupt local lymphatic drainage and contribute to the development of festoons. Although not specific to the periorbital region, studies have demonstrated that cosmetic procedures such as abdominal liposuction can significantly impact superficial lymphatic networks, leading to lymphatic stasis and potential postoperative complications—highlighting the broader relevance of lymphatic disruption in aesthetic interventions[17]. It is also important to ask about previous treatments, such as laser treatments, soft-tissue fillers, and botulinum toxin injections[18].
Physical Examination
A comprehensive physical examination is paramount in the evaluation of festoons, providing valuable insights into the characteristics of the swelling and helping to differentiate it from other potential causes of periorbital edema. Careful inspection of the skin texture, noting any signs of solar damage, such as wrinkles, fine lines, or actinic keratoses, can provide clues about the degree of photoaging contributing to the condition. Palpation of the affected area is essential to assess the consistency of the swelling, determine its borders, and identify any underlying masses or nodules. Assessment of facial symmetry is also crucial, as asymmetry may indicate underlying structural abnormalities or neuromuscular dysfunction.
Examination of the periorbital region should include assessment of the position and contour of the eyelids, noting any ptosis, ectropion, or entropion. A thorough evaluation should include assessment of the tear film and lacrimal drainage system, visual acuity in each eye, and extraocular muscle function.
Signs
The signs of festoons manifest as distinct clinical features that can be identified during physical examination. One of the most prominent signs is the presence of soft tissue swelling in the lower eyelids and cheeks, creating a puffy or bulging appearance. The skin overlying the festoons may exhibit characteristic changes, such as wrinkling, sagging, and a loss of elasticity. In some cases, the skin may appear erythematous or hyperpigmented, indicating chronic inflammation or sun damage. Additionally, festoons can cause a visible demarcation or crease between the lower eyelid and the cheek, accentuating the prominence of the swelling.
Symptoms
Patients with festoons may report a variety of symptoms, ranging from cosmetic concerns to functional impairments. Many individuals seek medical attention due to the aesthetic impact of festoons, describing feelings of being self-conscious or dissatisfied with their appearance. Some patients may experience a sensation of heaviness or pressure in the affected area, particularly in the lower eyelids, which can contribute to fatigue and discomfort. In severe cases, festoons can impair vision by obstructing the visual field or irritating the ocular surface. Similar to other orbital conditions involving anatomical distortion, patients may also report symptoms consistent with dry eye disease.[19].
Additionally, the psychological impact of festoons should not be underestimated.
Clinical Diagnosis
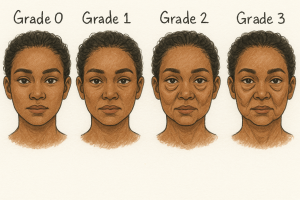
| Grade | Description |
|---|---|
| 0 | No festoon present |
| 1 | Mild festoon- minimal fullness or skin folds |
| 2 | Moderate festoon- noticeable fullness and skin folds |
| 3 | Severe festoon- substantial zygomatic fullness, distinct folds, possible discomfort |
The clinical diagnosis of festoons primarily relies on a comprehensive assessment of the patient's medical history, a thorough physical examination, and careful evaluation of the characteristic signs and symptoms. A detailed history should include inquiries about the onset, duration, and progression of the swelling, as well as any associated symptoms such as itching, pain, or visual disturbances. The clinician should also inquire about any potential contributing factors, such as sun exposure, smoking, allergies, or underlying medical conditions. During the physical examination, the clinician should carefully inspect the periorbital region, noting the size, shape, and location of the swelling, as well as any associated skin changes such as discoloration, texture irregularities, or telangiectasias. Palpation of the affected area can help assess the consistency of the swelling and identify any underlying masses or nodules.
Ruling out other potential causes of periorbital edema or facial swelling is essential for accurate diagnosis [2].
Safir et al. (2024) proposed a standardized clinical grading system to assess the severity of festoons. The scale ranges from Grade 0 to Grade 3, based on the degree of soft tissue fullness and skin folds in the lower eyelid and malar region:
Grade 0: No festoon present
Grade 1: Mild — minimal fullness or skin folds
Grade 2: Moderate — noticeable fullness and skin folds
Grade 3: Severe — pronounced zygomatic fullness with distinct skin folds; may be associated with discomfort
This grading system was used to evaluate treatment response to a thermal resurfacing drug delivery system with liquid tetracycline, demonstrating significant clinical and patient-reported improvements post-intervention [12].
Diagnostic Procedures
While the clinical diagnosis of festoons is primarily based on history and physical examination, certain diagnostic procedures may be employed to rule out other potential causes of facial swelling or to further evaluate the extent and characteristics of the condition. In some cases, imaging studies such as magnetic resonance imaging or computed tomography may be necessary to evaluate the underlying structures and rule out other potential causes of facial swelling, such as tumors, cysts, or vascular malformations. Skin biopsies may be considered in cases where the diagnosis is uncertain or when there are concerns about underlying skin pathology. In addition, tear film osmolarity, meibography, and Schirmer testing can be done.
It is important to recognize that diagnostic procedures play a complementary role in the evaluation of festoons.
Differential Diagnosis
The differential diagnosis of festoons encompasses a range of conditions that can cause periorbital edema or facial swelling, necessitating careful consideration and evaluation to ensure accurate diagnosis and management.
Allergic contact dermatitis can manifest with eyelid swelling, redness, itching, and scaling.
Angioedema characterized by rapid swelling of the skin and mucous membranes, may affect the periorbital region, often accompanied by urticaria or respiratory distress.
Transient malar edema presents as intermittent swelling in the cheek area, often exacerbated by factors such as sodium intake, hormonal fluctuations, or certain medications.
Thyroid Eye Disease (TED) can produce infraorbital fullness, but it is often accompanied by proptosis, lid retraction, extraocular motility restriction, and signs of orbital inflammation due to inflammation and enlargement of the extraocular muscles and orbital tissues. The malar region is usually spared, and the clinical course is often more progressive and asymmetric.
Blepharochalasis, a rare condition characterized by recurrent eyelid edema and subsequent atrophy of the eyelid skin, can mimic the appearance of festoons.
Orbital tumors or masses can cause proptosis, displacement of the globe, and periorbital swelling, necessitating imaging studies for evaluation.
Renal disease or heart failure may lead to fluid retention and generalized edema, including periorbital swelling.
Management
Festoons are a frequently occurring condition, yet treatment modalities are underrepresented in scientific literature[12].
Managing festoons effectively requires a multifaceted approach tailored to the individual patient's needs and preferences, encompassing both non-surgical and surgical interventions to address the underlying causes and aesthetic concerns[1].
More recently, non-surgical blepharoplasty techniques have emerged as alternatives for rejuvenating the periorbital area[20].
General Treatment
General treatment strategies for festoons focus on alleviating symptoms, improving aesthetic appearance, and addressing underlying contributing factors. Lifestyle modifications such as sun protection, smoking cessation, and avoidance of allergens can help minimize the progression and severity of festoons[1]. Topical corticosteroids or antihistamines may be prescribed to reduce inflammation and alleviate itching associated with festoons[1]. Manual lymphatic drainage, a gentle massage technique, can help improve lymphatic circulation and reduce fluid accumulation in the affected area.
Non-ablative laser treatments, such as radiofrequency or ultrasound therapy, can stimulate collagen production and improve skin elasticity, reducing the appearance of festoons[21].
Medical Therapy
Medical therapies for festoons primarily aim to address underlying inflammatory or allergic conditions that may contribute to their development and exacerbation. Topical corticosteroids may be prescribed to reduce inflammation and alleviate itching, while antihistamines can help control allergic reactions that may worsen festoons. The use of intralesional sclerotherapy—well-established in treating soft tissue masses like cystic hygromas—may offer a rationale for reducing festoons by targeting their characteristic soft tissue overgrowth[22]. Both tetracycline and doxycycline have demonstrated efficacy in reducing festoon and malar edema volume. Studies by Perry et al., Godfrey et al., and Chon et. al have shown significant improvement in contour and high patient satisfaction with minimal adverse effects [23][24][25]. The use of botulinum toxin injections to relax underlying muscles and potentially reduce the prominence of festoons has some theoretical basis, but the current evidence is limited and primarily focused on related applications. While there are well-established, approved applications for both functional and cosmetic purposes, ongoing research is exploring several additional off-label uses. [26].
Medical Follow-up
Medical follow-up is crucial for patients undergoing medical therapy for festoons, allowing for monitoring of treatment response, adjustment of medications as needed, and early detection of any potential complications. During follow-up visits, the clinician should assess the patient's symptoms, examine the periorbital region, and evaluate the effectiveness of the treatment regimen.
Surgery
Malar bags, palpebral bags, or festoons can be improved with the use of reliable surgical technique[27]. Surgical intervention remains the most effective approach for addressing festoons, offering the potential for significant and long-lasting improvement in both functional and aesthetic outcomes. Surgical excision has demonstrated success and is considered reliable, though it carries risks such as bleeding, symptom aggravation, partial resection, and recurrence[5][28]. Various surgical techniques can be employed, including direct excision, blepharoplasty, and midface lift, each with its own advantages and limitations. Direct excision involves the surgical removal of the excess skin and subcutaneous tissue, while blepharoplasty techniques can also be used. Midface lift procedures can elevate the cheek and reposition the soft tissues, improving the contour of the lower eyelid and reducing the appearance of festoons. Surgical intervention is often pursued after conservative methods prove insufficient[29]. Careful preoperative planning and patient selection are essential to optimize surgical outcomes and minimize the risk of complications.
Surgical Follow-up
Following surgical intervention for festoons, meticulous postoperative care and regular follow-up visits are essential to ensure optimal healing, minimize complications, and maximize long-term outcomes. Postoperative instructions typically include wound care, pain management, and activity restrictions to promote healing and prevent infection[30][31]. Patients should be educated on the signs and symptoms of infection, hematoma formation, and other potential complications, and instructed to seek prompt medical attention if any concerns arise.
During follow-up visits, the surgeon should assess the surgical site for proper healing, monitor for any signs of complications, and evaluate the aesthetic outcome of the procedure.
Complications
Although surgical intervention can significantly improve the appearance of festoons, it is important to recognize the potential for complications, which can range from minor and self-limiting to more severe and may require additional intervention. Common complications include hematoma formation, infection, wound dehiscence, asymmetry, contour irregularities, and scarring[32]. Ectropion, or the outward turning of the eyelid, can occur if excessive skin is removed or if the eyelid support structures are weakened during surgery[33][5][2]. In some cases, patients may experience changes in sensation or numbness in the periorbital region, which may be temporary or permanent. [34]
Prognosis
The prognosis for festoons varies depending on the underlying cause, severity, individual patient factors, and the therapeutic approach to the disease. With appropriate management, including lifestyle modifications, medical therapies, and surgical intervention, many patients can experience significant improvement in their symptoms and aesthetic appearance. Primary intervention, early intervention and adherence to treatment recommendations can help prevent the progression of festoons and minimize their impact on quality of life.
Additional Resources
American Society of Ophthalmic Plastic and Reconstructive Surgery is a professional organization dedicated to advancing the field of ophthalmic plastic and reconstructive surgery, providing resources and education for both physicians and patients. (ASOPRS) https://asoprs.org/
The American Academy of Ophthalmology offers comprehensive information on various eye conditions, including festoons, as well as educational materials and resources for patients and healthcare professionals. https://www.aao.org/
References
- ↑ 1.0 1.1 1.2 1.3 Chon BH, Hwang CJ, Perry JD. Treatment Options for Lower Eyelid Festoons. Facial Plastic Surgery Clinics of North America. 2021;29(2):301. doi:10.1016/j.fsc.2021.02.005
- ↑ 2.0 2.1 2.2 2.3 Kpodzo D, Nahai F, McCord CD. Malar Mounds and Festoons. Aesthetic Surgery Journal. 2014;34(2):235. doi:10.1177/1090820x13517897
- ↑ Asaadi M, Gazonas CB, Didzbalis CJ, Colon A, Tran BN. Outcomes of Surgical Treatment of Malar Mounds and Festoons. Aesthetic Plastic Surgery. 2023;47(4):1418. doi:10.1007/s00266-023-03381-4
- ↑ Žgaljardić Z, Žgaljardić I, Jurić F. Treatment of malar mound and festoon with fractional microneedle bipolar radiofrequency combined with 15% TCA peel. Journal of Cosmetic Dermatology. 2020;20(6):1810. doi:10.1111/jocd.13740
- ↑ 5.0 5.1 5.2 Gupta LY, Gupta SS, Bamberger JN, Gupta KR. Mini-Incision Direct Festoon Access, Cauterization, and Excision (MIDFACE): A 12-Year Analysis of a Novel Festoon Surgery. Plast Reconstr Surg. 2023;152(5):987-999. doi:10.1097/PRS.0000000000010365
- ↑ Dai G, Freudenberger T, Zipper P, et al. Chronic ultraviolet B irradiation causes loss of hyaluronic acid from mouse dermis because of down-regulation of hyaluronic acid synthases. Am J Pathol. 2007;171(5):1451-1461. doi:10.2353/ajpath.2007.070136
- ↑ Koh JS, Kang H, Choi SW, Kim HO. Cigarette smoking associated with premature facial wrinkling: image analysis of facial skin replicas. Int J Dermatol. 2002;41(1):21-27. doi:10.1046/j.1365-4362.2002.01352.x
- ↑ Czajkowska J, Juszczyk J, Bugdol M, et al. High-frequency ultrasound in anti-aging skin therapy monitoring. Scientific Reports. 2023;13(1). doi:10.1038/s41598-023-45126-y
- ↑ McCullough JL, Kelly KM. Prevention and Treatment of Skin Aging. Annals of the New York Academy of Sciences. 2006;1067(1):323. doi:10.1196/annals.1354.044
- ↑ Safa M, Natalizio A, Hee CK. A Prospective, Open-Label Study to Evaluate the Impact of VYC-12L Injection on Skin Quality Attributes in Healthy Volunteers. Clinical Cosmetic and Investigational Dermatology. Published online March 1, 2022:411. doi:10.2147/ccid.s352007
- ↑ Scallan JP, Huxley VH, Korthuis RJ. Pathophysiology of Edema Formation. Published online January 1, 2010. Accessed May 2025. https://www.ncbi.nlm.nih.gov/books/NBK53445/
- ↑ 12.0 12.1 12.2 12.3 Safir M, Waizer I, Safir A, Hartstein ME, Artzi O. Percutaneous delivery of liquid tetracycline using a thermal resurfacing drug delivery system for the treatment of festoons. Lasers in Surgery and Medicine. 2024;56(5):454. doi:10.1002/lsm.23786
- ↑ Moradi A, Montes JR, Humphrey S, et al. A Unified Approach to Facial Contours and Volume Correction: The Role of the Cheek and the Chin. Plastic & Reconstructive Surgery Global Open. 2024;12(10). doi:10.1097/gox.0000000000006219
- ↑ Newberry CI, Mccrary H, Thomas JR, Cerrati EW. Updated Management of Malar Edema, Mounds, and Festoons: A Systematic Review. Aesthet Surg J. 2020;40(3):246-258. doi:10.1093/asj/sjz137
- ↑ Genovese L, Corbo A, Sibilla S. An Insight into the Changes in Skin Texture and Properties following Dietary Intervention with a Nutricosmeceutical Containing a Blend of Collagen Bioactive Peptides and Antioxidants. Skin Pharmacol Physiol. 2017;30(3):146-158. doi:10.1159/000464470
- ↑ Kim DU, Chung HC, Choi J, Sakai Y, Lee BY. Oral Intake of Low-Molecular-Weight Collagen Peptide Improves Hydration, Elasticity, and Wrinkling in Human Skin: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients. 2018;10(7):826. Published 2018 Jun 26. doi:10.3390/nu10070826
- ↑ Marxen T, Shauly O, Goel P, Tsan T, Faria R, Gould DJ. The Utility of Lymphatic Massage in Cosmetic Procedures. Aesthet Surg J Open Forum. 2023;5:ojad023. Published 2023 Feb 28. doi:10.1093/asjof/ojad023
- ↑ Ahn CS, Davis SA, Dabade TS, Williford PM, Feldman SR. Cosmetic procedures performed in the United States: a 16-year analysis. Dermatol Surg. 2013;39(9):1351-1359. doi:10.1111/dsu.12267
- ↑ Yu Y, Hu YX, Lu MX, et al. Risk Factors for Ocular Surface Irritation Symptoms in Inactive Mild and Moderate-to-Severe Graves' Orbitopathy. Ophthalmol Ther. 2024;13(4):1015-1024. doi:10.1007/s40123-024-00892-4
- ↑ Miotti G, Zeppieri M, Pederzani G, Salati C, Parodi PC. Modern blepharoplasty: From bench to bedside. World Journal of Clinical Cases. 2023;11(8):1719. doi:10.12998/wjcc.v11.i8.1719
- ↑ Endara M, Oh C, Davison SP, Baker SB. The Management of Festoons. Clinics in Plastic Surgery. 2014;42(1):87. doi:10.1016/j.cps.2014.08.006
- ↑ Kumar N, Kohli M, Pandey S, Tulsi SP. Cystic hygroma. Natl J Maxillofac Surg. 2010;1(1):81-85. doi:10.4103/0975-5950.69152
- ↑ Perry JD, Mehta VJ, Costin BR. Intralesional tetracycline injection for treatment of lower eyelid festoons: a preliminary report. Ophthalmic Plast Reconstr Surg. 2015;31(1):50-52. doi:10.1097/IOP.0000000000000173
- ↑ Godfrey KJ, Kally P, Dunbar KE, et al. Doxycycline Injection for Sclerotherapy of Lower Eyelid Festoons and Malar Edema: Preliminary Results. Ophthalmic Plast Reconstr Surg. 2019;35(5):474-477. doi:10.1097/IOP.0000000000001332
- ↑ Chon BH, Hwang CJ, Perry JD. Long-Term Patient Experience with Tetracycline Injections for Festoons. Plast Reconstr Surg. 2020;146(6):737e-743e. doi:10.1097/PRS.0000000000007334
- ↑ Campanati A, Martina E, Giuliodori K, Consales V, Bobyr I, Offidani A. Botulinum Toxin Off-Label Use in Dermatology: A Review. Skin Appendage Disord. 2017;3(1):39-56. doi:10.1159/000452341
- ↑ Höenig JF, Knutti D, Fuente A de la. Vertical Subperiosteal Mid-face-lift for Treatment of Malar Festoons. Aesthetic Plastic Surgery. 2011;35(4):522. doi:10.1007/s00266-010-9650-3
- ↑ Chu RL, Godbe K, Sciulli HD, Krachmalnick SJ, Abdo M, Sokol JA. More Than Under-Eye Bags: Treatment of Formidable Festoons. Ophthalmic Plast Reconstr Surg. 2025;41(1):e1-e2. doi:10.1097/IOP.0000000000002769
- ↑ Paolo F, Fallico N, Parisi P, Scuderi N. Periorbital area rejuvenation using carbon dioxide therapy. Journal of Cosmetic Dermatology. 2012;11(3):223. doi:10.1111/j.1473-2165.2012.00633.x
- ↑ Mathijssen IMJ, Meulen JC van der. Guidelines for reconstruction of the eyelids and canthal regions. Journal of Plastic Reconstructive & Aesthetic Surgery. 2009;63(9):1420. doi:10.1016/j.bjps.2009.05.035
- ↑ Park R, Akella SS, Aakalu VK. A review of surgical management of progressive myogenic ptosis. Orbit. 2022;42(1):11. doi:10.1080/01676830.2022.2122514
- ↑ Botti G, Botti C, Fabbri M, et al. Direct Excision of Malar Bags: Back to the Basics. Aesthetic Plast Surg. 2024;48(21):4307-4313. doi:10.1007/s00266-024-04411-5
- ↑ Rames JD, Rames MM, Yu CY, et al. Risk Factors for Ectropion After Lower Eyelid and Cheek Reconstruction Following Mohs Micrographic Surgery. Plast Reconstr Surg Glob Open. 2025;13(2):e6498. Published 2025 Feb 3. doi:10.1097/GOX.0000000000006498
- ↑ Ziegler UE, Schäfer RC, Daigeler A, Zeplin PH. Extending the Indications for Direct Transcutaneous Lower Blepharoplasty With an Infraorbital Incision to Tear Trough Deformities, Suborbicularis Oculi Fat, Festoons, and Revision Blepharoplasty. Plast Surg (Oakv). 2024;32(3):499-507. doi:10.1177/22925503221120545