Cotton Wool Spots
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
In otherwise healthy patients, the observance of a cotton-wool spot is not considered normal. A single cotton-wool spot in one eye can be the earliest ophthalmoscopic finding in diabetic retinopathy or hypertensive retinopathy. In a series of patients who had cotton-wool spots and no known medical history, diastolic blood pressure ≥90 mm Hg was detected in 50% of patients and elevated blood sugar was found in 20% of patients.[1] [2] [3]
Etiology[2][3][4] [5]
Cotton-wool spots have many different etiologies:
- Ischemic: Hypertension, diabetes, ocular ischemic syndrome, retinal vein occlusion, anemia, hyperviscosity state, hypercoagulable state, radiation, acute blood loss
- Immune and inflammatory conditions: Systemic lupus erythematosus, dermatomyositis, scleroderma, polyarteritis nodosa, giant cell arteritis
- Infectious: HIV retinopathy, cat-scratch disease, Rocky Mountain spotted fever, leptospirosis, onchocerciasis, bacteremia, fungemia
- Embolic: carotid emboli, cardiac emboli, cardiac valvular disease, endocarditis, rheumatic heart disease, deep venous emboli, Purtscher-like retinopathy, foreign-body emboli
- Neoplastic: lymphoma, leukemia, metastasis
- Medication-induced: interferon retinopathy
- Miscellaneous: trauma, epiretinal membrane, high-altitude retinopathy, papilledema, papillitis, Purtscher retinopathy.
- Idiopathic
Pathophysiology
Cotton-wool spots are believed to occur secondary to ischemia from retinal arteriole obstruction.[5] They are thought to represent nerve fiber layer infarct and pre-capillary arteriolar occlusion. However, factors responsible for focal interruption of axoplasmic flow in the retinal nerve fiber layer may result in similar intra-axonal organelle accumulations.[6]
The histologic hallmark of cotton-wool spots is considered by many to be cytoid bodies, so named because they look like cells though they are eosinophilic segments of ganglion cell axons that are swollen because of defective axoplasmic flow. Cytoid bodies are usually packed with accumulations of mitochondria and other intracellular material.[7] [8]
Diagnosis
Signs
On ophthalmic fundus exam, cotton-wool spots may appear as small, yellow-white (or grayish-white), slightly elevated lesions, which look like clouds with a fimbriate border in the superficial retina. Usually they are less than one-third disc area in diameter, and are commonly found in the posterior pole of the fundus.[5]
Symptoms
In general, cotton-wool spots are visually asymptomatic; however, a patient may present with vision loss if the fovea is involved.[5] Systemic symptoms of the underlying etiology may be present.
Clinical Diagnosis

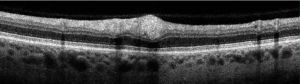
Diagnosis is usually made following a complete ocular examination, including a detailed dilated fundus exam. However, fluorescein angiography may reveal areas of capillary nonperfusion adjacent to cotton-wool spots.[1] Additional workup may be needed to detect the underlying etiology. On optical coherence tomography (OCT), cotton-wool spots can appear as focal or segmental areas of thickening, with hyperreflectivity of the inner retinal layers in the acute phase. This thickening may be mostly confined to the nerve fiber layer with sparing of the outer retinal layers, consistent with the postulation of axoplasmic debris accumulation within the ganglion cell axons that correlate to clinically apparent cotton-wool spots.[9] During resolution, these lesions can progress to inner retinal thinning or atrophy, or may in some cases result in cystic changes. Optical coherence tomography has been used to monitor the progression, extent, and resolution of cotton-wool spots.
Differential Diagnosis
Differential diagnosis of other yellow-white retinal lesions may include myelinated nerve fibers, hard exudate, retinal infiltrate, retinitis, retinal drusen, chorioretinal atrophy, intraluminal plaque,and early endogenous chorioretinitis.[10]
Management
Workup and treatment are directed towards the underlying etiology. Cotton-wool spots usually disappear in 6–12 weeks; however, they may persist for longer in patients with diabetic retinopathy.[1][5] While cotton-wool spots are a hallmark of retinopathy related to human immunodeficiency virus (HIV) infection, the presence of new or large cotton-wool spots should be monitored closely if the CD4 count is <200, as this may represent an early sign of viral retinitis.[11]
Initial workup may include vitals (blood pressure, heart rate, etc.) metabolic panels (e.g., glycosylated hemoglobin), complete blood count, and HIV testing. Directed workup may include an echocardiogram, electrocardiogram, and carotid ultrasound, and measuring erythrocyte sedimentation rate, C-reactive protein, other proteins), prothrombin time/partial thromboplastin time, and homocysteine.
Additional Resources
- Porter D. Blood pressure. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/blood-pressure-list. Published February 27, 2018. Accessed June 10, 2025.
References
- ↑ 1.0 1.1 1.2 Gerstenblith AT, Rabinowitz MP, Barahimi BI et al, eds. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 6th ed. Lippincott Williams & Wilkins; 2012.
- ↑ 2.0 2.1 Brown GC, Brown MM, Hiller T, et al. Cotton-wool spots. Retina. 1985;5(4):206-214.
- ↑ 3.0 3.1 Arroyo JG. Cotton-wool spots may challenge diagnosis. Rev Ophthalmology. 2004:111-114.
- ↑ Arroyo JG, Irvine AR. Retinal distortion and cotton-wool spots associated with epiretinal membrane contraction. Ophthalmology. 1995;102(4):662-668.
- ↑ 5.0 5.1 5.2 5.3 5.4 Patel PS, Sadda SR. Retinal artery obstructions. In: Ryan SJ, ed. Retina. 5th ed. Elsevier;2012: 1012-1025.
- ↑ McLeod D, Marshall J, Kohner EM, et al. The role of axoplasmic transport in the pathogenesis of retinal cotton-wool spots. Br J Ophthalmol. 1977;61(3):177-191.
- ↑ McLeod D. Why cotton wool spots should not be regarded as retinal nerve fibre layer infarcts. Br J Ophthalmol. 2005;89(2):229-237.
- ↑ Eagle RC Jr. Eye Pathology: An Atlas and Text. 2nd ed. Lippincott Williams & Wilkins; 2011.
- ↑ Ioannides A, Georgakarakos ND, Elaroud I, et al. Isolated cotton-wool spots of unknown etiology: management and sequential spectral domain optical coherence tomography documentation. Clin Ophthalmol. 2011;5:1431-1433.
- ↑ The Eyes Have It: Yellow-White Things in the Retina. http://www.aao.org/theeyeshaveit/optic-fundus/yellow-white.cfm (accessed 11 02, 2014).
- ↑ Chen C, Guo CG, Meng L, et al. Comparative analysis of cytomegalovirus retinitis and microvascular retinopathy in patients with acquired immunodeficiency syndrome. Int J Ophthalmol. 2017;10(9):1396-1401.