Conjunctival Myxoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Conjunctival myxoma is a rare, benign tumor of mesenchymal origin that arises from the conjunctiva. It typically presents as a slow-growing, painless, gelatinous or cystic mass on the bulbar conjunctiva, often in the temporal region. Although generally isolated and benign, its presence can be associated with systemic conditions like Carney complex, necessitating further systemic evaluation. Histopathology reveals spindle or stellate cells within a myxoid stroma. Complete surgical excision is the treatment of choice, with low risk of recurrence.
Disease Entity
Disease
Conjunctival myxoma is an extremely rare, benign tumor of mesenchymal origin, first described in 1913 by Magalif [1][2][3]. These tumors typically present as gelatinous, translucent, well-circumscribed, and painless masses that tend to grow slowly[3][2][4][5]. Ocular myxomas have also been reported in other parts of the eye, including the orbit, optic nerve, cornea, eyelid, and the lacrimal glands [4]. Conjunctival myxomas mainly affect adults, with a reported mean age of 45.1 - 47.6 years, without clear sex predilection or racial predisposition[2][6][7]. These tumors account for <0.001% to 0.16% of all conjunctival lesions according to several studies [3][7].
Etiology & Risk Factors
Conjunctival myxomas commonly occur as localized, isolated lesions[3][6]. These rare, benign tumors are derived from primitive fibroblastic mesenchymal cells and arise from the substantia propria of the conjunctiva [2][6]. In rare presentations, conjunctival myxomas have been noted as components of systemic manifestations including Carney complex or the mutations associated with it in PRKAR1A gene, as well as Zollinger-Ellison syndrome [5][7][8][9].
No association with trauma or family history has been reported by patients[4] [6][10]. However, in some cases, a history of foreign body injuries within the affected eye or prior surgeries at the site of the lesion, including cataract, strabismus, and epiblepharon surgeries, were reported by some patients[4] [10]. To date, no exact etiological trigger has been reported in the literature, and no definitive risk factors have been identified [7].
General Pathology
Conjunctival myxomas on gross examination are typically soft and smooth, with a semi-translucent to translucent appearance, and white, pink, or fleshy color. Characteristics of these tumors include presenting as solid, gelatinous, and well-circumscribed masses [2][4][6]. No hemorrhage, calcifications, and necrosis have been reported [6]. Dimensions of conjunctival myxomas range from 1 mm to 30 mm [7].
Histopathology
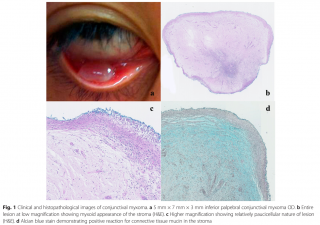
Conjunctival myxomas are benign tumors derived from primitive mesenchymal cells [7]. They originate from Tenon’s capsule and extend to the substantia propria [7], under the cover of conjunctival epithelium [1][6]. Microscopically, these tumors are typically composed of a small number of spindle- and stellate-shaped cells scattered within loose myxoid stroma rich in hyaluronic acid [2][3], with minimal vascular structures, delicate reticulin fibers passing in various directions, as well as mature, wavy, and thin collagen fibers [5][11][12]. The myxoid stroma shows diffuse positive staining for connective tissue mucin with Alcian blue and colloidal iron stains [4][6][9]. Digested Periodic-acid-Schiff (PAS) staining was negative for epithelial mucin[10]. (Figure 1)
Immunohistochemical Findings
Conjunctival myxomas are positive for vimentin, and most cases show strong immunoreactivity for CD34. These tumor cells are negative for S100 protein and α-SMA, and they also lack immunoreactivity for SRY-Box Transcription Factor 10, desmin, myoglobin, epithelial membrane antigen, lysozyme and cytokeratin [4][6].
Pathophysiology
Conjunctival myxomas are benign tumors derived from primitive fibroblastic mesenchymal cells as confirmed by histopathological and immunohistochemical findings [2][6], since these tumors are positive for vimentin and CD34, with negative immunoreactivity to S100 protein and α-SMA, which indicates their mesenchymal origin [4][6][9]. They develop within the substantia propria layer of the conjunctiva and are usually covered by conjunctival epithelium [1][6][7]. The pathogenesis of conjunctival myxomas is not fully understood yet, due to their extreme rarity and limited cases reported[4]. The mechanism of the slowly growing and non-tender nature of conjunctival myxomas is not clear, but it’s likely due to their benign histology suggesting that their growth is due to matrix expansion rather than aggressive cellular proliferation.
These tumors typically occur as isolated lesions without metastasis [6]. However, conjunctival myxomas can be associated with Zollinger-Ellison syndrome, which includes or constitute a component of the Carney complex, which is an autosomal dominant syndrome associated with cardiac and cutaneous myxomas, pigmented lesions, and endocrine overactivity dysfunction [4][6]. Conjunctival myxomas have not been reported with other systemic diseases associated with myxomas, such as Mazabraud syndrome or McCune-Albright syndrome [10].
Primary Prevention
There are currently no defined preventive measures for conjunctival myxomas, due to the lack of a clear etiology or any modifiable, behavioral, or environmental risk factors [7].
Diagnosis
Conjunctival myxomas can be mistaken for other tumors and lesions including, amelanotic nevus, amelanotic melanoma, lipoma, squamous cell carcinoma, conjunctival cyst, lymphangioma, and neurofibroma [3][6][10].
Complete excisional biopsy with histopathological analysis are required to confirm the diagnosis [4][5]. Key histological features of conjunctival myxomas include spindle- and stellate-shaped cells scattered within loose myxoid stroma, which contains minimal blood vessels, delicate reticulin fibers, and mature collagen fibers [5]. Immunohistochemical staining shows that this tumor is positive for vimentin and CD34 but negative for α-SMA and S100. These findings support the diagnosis of conjunctival myxoma [4][6][9].
On ultrasound biomicroscopy, conjunctival myxomas show dome-shaped subepithelial masses, which are characterized by homogeneously low internal reflectivity and hypoechogenic foci, indicating internal vascularization. High-resolution optical coherence tomography (HR-OCT) is usually helpful in distinguishing conjunctival myxoma from similar conjunctival lesions [7].Systemic evaluation is recommended if conjunctival myxoma is confirmed, taking into consideration the possible association with Carney complex and Zollinger-Ellison syndrome [2][4].
History
Most patients report a gradually enlarging, painless swelling within the conjunctiva, persisted over a period of weeks to years. In most cases, conjunctival myxomas are discovered incidentally. Most conjunctival myxoma cases are not associated with history of trauma, discharge, redness, eye surgeries, or family history of similar ocular lesions [1][3][4][5][6][10][13]. However, a few atypical cases have been reported with a history of prior eye surgeries, as well as associated redness, tearing, and pain[2] [3][9][14].
Physical Examination
Physical and ocular examinations of most conjunctival myxoma patients are unremarkable [6]. Typically, slit-lamp examination reveals a well-circumscribed, elevated, non-tender, and translucent mass, ranging in size from 1 mm to 30 mm in diameter [5][7][8]. These tumors may be unencapsulated or partially encapsulated. In rare cases, patients may present with minimal ocular motility restriction or decreased visual acuity[1][6][7][8][13].
Signs
Most conjunctival myxoma patients present with a solitary, unilateral, localized, and gelatinous mass [4][7][15]. These tumors may appear with fleshy, white, yellow, pale or pink to salmon pink in color [5][7][9]. Majority of conjunctival myxoma lesions have been reported in the temporal conjunctiva, followed by nasal conjunctiva as the second most common site , with a lesser number of cases occurring within other conjunctival locations[7].
Symptoms
Most patients with conjunctival myxoma are typically asymptomatic [3][6][7][10]. Patients are present after visually noticing the lesion [1][4][15]. Rarely, discomfort sensation is reported [5][10]. Symptoms such as pain, redness and discharge are rarely documented [1][3][9][14].
Clinical Diagnosis
The Clinical Diagnosis of Conjunctival Myxoma is challenging due to its rarity. It is commonly misdiagnosed as other Clinical tumors. Pearls that Aid in clinical diagnosis include a painless, slow-growing, gelatinous or translucent subconjunctival mass, pinkish yellow in color, commonly found in the bulbar conjunctiva [16][17][18]. As it may be confused with other clinical etiologies. Diagnosis relies on histopathological examination, which shows stellate and spindle-shaped cells embedded in hyaluronidase-rich mucin. Typically, they stain positive for vimentin, CD34, and smooth muscle. actin. Most of the lesions stain negative for S-100[17][18]. Imaging modalities such as anterior segment optical coherence tomography (AS-OCT) or ultrasound biomicroscopy (UBM) may aid in assessing lesion depth and extension.
Diagnostic Procedures
The diagnosis of conjunctival myxoma requires a combination of clinical evaluation, imaging, and, most importantly, histopathological analysis. AS-OCT and UBM can help delineate the lesion's depth and extent, helping distinguish it from cystic or solid tumors[17]. Typically, a patient with the lesion will undergo wide local excision with margin assessment, which is critical for diagnosis. Histopathological examination shows spindle-shaped fibroblasts within a mucinous stroma that stains positively for Alcian blue (hyaluronidase-sensitive) and vimentin, with variable CD34 expression. Immunohistochemistry helps differentiate myxoma from other myxoid lesions, such as myxoid neurofibroma or metastatic mucinous adenocarcinoma[17]. Additionally, due to its rare association with Carney complex, a systemic evaluation including cardiac and endocrine screening may be warranted in recurrent or multifocal cases[19].
Laboratory Test
Conjunctival myxoma is primarily diagnosed through histopathological examination, as there are no specific laboratory tests to confirm the tumor. However, additional tests may support the diagnosis and rule out systemic associations. Testing is done when Carney complex is suspected, genetic testing for PRKAR1AS mutation, endocrine screening (ex: cortisol, growth hormone) may be warranted, as part of the Carney complex involves endocrine hyperactivity secondary to tumors . Systematic evaluation including echocardiography is recommended to exclude cardiac myxomas, which are the hallmark of Carney syndrome.
Differential Diagnosis
Several benign and malignant lesions present similarly to conjunctival myxoma due to their overlapping features. These include, conjunctival cyst, lymphangioma, myxoid neurofibroma, and amelanotic nevi or melanoma. These conditions can be differentiated based on their histopathological features [17]. Conjunctival lymphangiectasia, these appear as a clear, fluid-filled channels but lacks solid stromal components, and are highly vascularized, whereas myxomas are not. Conjunctival cysts are typically unilocular and transilluminate brightly. . Myxoid neurofibromas are not cystic, and they exhibit spindle-shaped nuclei and wavy collagen bundles that are often associated with systemic neurofibromatosis, and they demonstrate S-100 positivity on immunohistochemistry [16] [17]. Unlike conjunctival amelanotic nevi and melanomas, which are characterized by prominent intrinsic vascularity or pigmentation, myxomas do not have these features[17][18].
Management
Conjunctival myxoma is primarily a surgical disease, with no established first-line medical therapy.
Surgery
The primary treatment of conjunctival myxoma is complete surgical excision with clear margins, to prevent recurrence [16][17]. Incomplete removal may lead to regrowth [16]. The tumor’s gelatinous consistency makes careful dissection essential, often aided by frozen section control to ensure complete resection. It has a recurrence rate of 15-30% incases with incomplete resection[16].
Surgical Follow-up
Long term follow up is recommended due to the potential for local recurrence. Recurrence is commonly attributed to incomplete excision, tumor multicentricity, or a genetic predisposition.
Complications
Local complications include recurrence, conjunctival scarring & symblepharon, and conjunctival defects. Systemic complications are commonly due to the rare association with Carney Complex, and these include Cardiac Myxoma, which are life threatening, and they occur in about 30% of Carney complex patients[19].
Prognosis
Conjunctival Myxoma is a benign tumor with an excellent prognosis following surgical excision. Most recurrences occur within 2 years, necessitating the need for long term follow up [16]. Systemic prognosis depends on associations: sporadic cases have no long-term risks, while Carney complex-associated myxomas require lifelong surveillance for cardiac myxomas (potentially fatal if untreated) and endocrine tumors.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Pandey, Jayati & Khan, Perwez & Khan, Lubna & Srivastava, Ankita & Ranjan, Alok. (2020). Conjunctival myxoma: A case report in northern India. Indian Journal of Clinical and Experimental Ophthalmology. 6. 645-647. 10.18231/j.ijceo.2020.136.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Hung KH, Yeh LK. Clinical appearance and pathological findings of conjunctival myxoma: Case report and literature review. Am J Ophthalmol Case Rep 2020;19:100860.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Kini Rao AC, Nayal B. Conjunctival myxoma-a case report. Malays J Med Sci 2013;20(1):92–94.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 Lee SE, Lee SB, Kim K, Sung JY. Conjunctival myxoma: A case report and review of a rare tumor. Medicine 2024;103(10):e37342.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Alkharashi M, Alkatan HM, Alhumidi AA, Otaif W. Conjunctival myxoma masquerading as conjunctival lymphoma: A case report. Int J Surg Case Rep 2022;97:107441.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 Xiong MJ, Dim DC. Conjunctival myxoma: A synopsis of a rare ocular tumor. Arch Pathol Lab Med 2015;139(5):693–697.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 7.15 Najdawi W, Li WJ, De Arrigunaga S, et al. Subepithelial lesions of the ocular surface: A review. Curr Ophthalmol Rep 2025;13:8.
- ↑ 8.0 8.1 8.2 Park ES, Kim MS, Jun I, Kim TI, Seo KY. A rare case of conjunctival myxoma initially misdiagnosed as a conjunctival inclusion cyst. Korean J Ophthalmol 2021;35(5):419–420.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Chen YP, Tsung SH, Lin TY. A rare presentation of conjunctival myxoma with pain and redness: case report and literature review. Case Rep Ophthalmol 2012;3(1):145–150.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 Sharma N, O’Hagan S, Phillips G. Conjunctival myxoma – atypical presentation of a rare tumour: case report and review of literature. BMC Ophthalmol 2016;16:54.
- ↑ Ríos Y Valles-Valles D, Hernández-Ayuso I, Rodríguez-Martínez HA, Medina-Cruz A, Salcedo-Casillas G, Rodríguez-Reyes AA. Primary conjunctival myxoma: case series and review of the literature. Histopathology 2017;71(4):635–640.
- ↑ Milman T, Salomao DR, Ida CM, Capiz Correa DR, Grossniklaus HE, Zhang Q, Hamershock RA, Shields C, Shields JA, Raber I, Rapuano CJ, Patel R, Eagle RC. Conjunctival myxoid lesions: Clinical-pathologic multiparametric analysis, including molecular genetics (An American Ophthalmological Society thesis). Am J Ophthalmol 2019;205:115–131.
- ↑ 13.0 13.1 Mehta S, Natarajan R. A rare case of conjunctival myxoma: Putting diagnostic tests and prognostic factors into perspective. J Cornea Ocul Surface 2023;1(1):67–70.
- ↑ 14.0 14.1 Feng PW, Herskowitz WR, Tang V, Khzam RA, Dubovy SR, Galor A, Karp CL. Characteristics of conjunctival myxomas on anterior segment optical coherence tomography. Can J Ophthalmol 2024;59(6):e865–e871.
- ↑ 15.0 15.1 Pe'er J, Hidayat AA. Myxomas of the conjunctiva. Am J Ophthalmol 1986;102:80–86.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Lee, S.E. et al. (2024) ‘Conjunctival Myxoma: A case report and review of a rare tumor’, Medicine, 103(10). doi:10.1097/md.0000000000037342.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 Alvarado-Villacorta, R. et al. (2022) ‘Conjunctival Myxoma: A systematic review of a rare tumor’, Survey of Ophthalmology, 67(3), pp. 729–740. doi:10.1016/j.survophthal.2021.08.007.
- ↑ 18.0 18.1 18.2 Demirci, H. (2006) ‘Report of a conjunctival myxoma case and review of the literature’, Archives of Ophthalmology, 124(5), p. 735. doi:10.1001/archopht.124.5.735.
- ↑ 19.0 19.1 Kennedy, R.H. et al. (1991) ‘The Carney complex with ocular signs suggestive of cardiac myxoma’, American Journal of Ophthalmology, 111(6), pp. 699–702. doi:10.1016/s0002-9394(14)76773-x.