Coats Disease
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Coats disease is a telangiectatic neovascular disease of the retina of unknown etiology. It usually affects one eye rather than both eyes.
In 1908, George Coats described the histopathologic features of enucleated eyes with massive exudations.[1] He divided the morphology into 3 groups[2] :
- Group I: massive subretinal exudate alone
- Group II: massive subretinal exudate, intraretinal and subretinal hemorrhage, and retinal vascular dilatations
- Group III: subretinal exudate and retinal arteriovenous malformations. Later, Eugen von Hippel recognized group III as a separate entity, called angiomatosis retinae
Based on a large study of 117 patients, the 2000 Proctor Lecture defined Coats disease as 'idiopathic retinal telangiectasia and intraretinal or subretinal exudation without appreciable signs of vitreoretinal traction."[3]
Disease Entity
Coats disease is characterized by unilateral (95%), progressive development of abnormal vessels in the retina of the affected individuals. It’s more frequent in males (at least 3:1) than females, and is seen most often in patients aged <8 years, though it has been observed in both infants and older patients. It is primarily caused by aneurysms and telangiectatic vessels within the temporal retina. These abnormal vessels are leaky and there is exudation in various degrees.
Other names
Leber's miliary aneurysm is considered to be a milder variant of Coats disease, and is generally not associated with massive subretinal exudation, hemorrhage, or exudative retinal detachment. Type 1 idiopathic macular telegiectasia is now considered to be the same as Coats disease.[2]
Genetics
No genetic basis for Coats disease has been positively identified, but chromosomal instability in chromosomes 3 and 13 has been posited as one cause.
Other genes which have been implicated include:
- Norrie Disease Pseudoglioma gene
- CRB1
- PANK2
Associations
Coats disease–like responses have been noted in cases of patients with Turner syndrome, Senior Loken syndrome, retinitis pigmentosa (both syndromic and isolated), facioscapulohumeral dystrophy (FSHD), and linear scleroderma/Parry Romberg syndrome. In females, bilateral involvement and FSHD should be ruled out.
Diagnosis
Signs and Symptoms
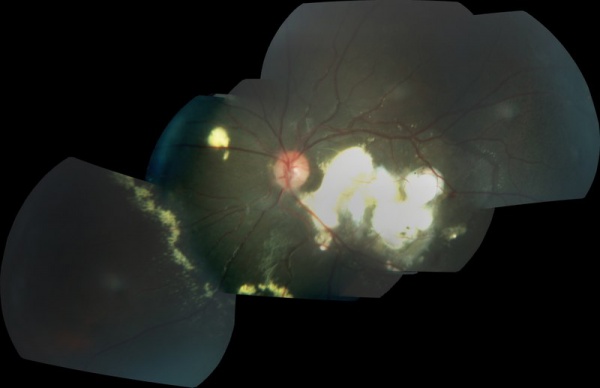
In a retrospective case series of 150 patients with Coats disease, the most common first symptoms were decreased visual acuity (34%) and strabismus (23%). In 76% of eyes, visual acuity at presentation was 20/200 to finger counting or hand motions to no light perception. While the anterior segment was normal in 90% of eyes, in all but 2 eyes the retinal telangiectasia involved the midperipheral or peripheral fundus. Retinal exudation was present in all 12 clock hours in 55% of eyes and ≥6 clock hours in 73%) of eyes. Ultrasonography typically showed a retinal detachment but no solid mass.[4]
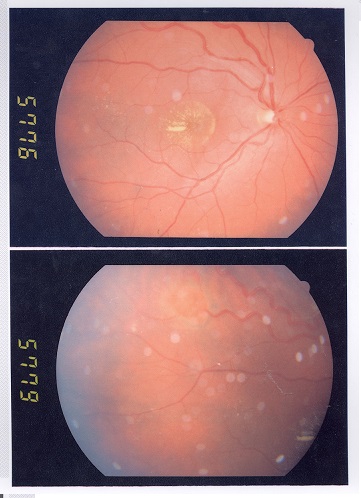
In mild cases, 1 or 2 foci of retinal telangiectasia may be found on the temporal hemispheres. Microaneurysms and thickening of retinal vessels are seen. Affected vessels show irregular enlargement with aneurysms which light up during fluorescein angiography.
Vascular abnormalities are usually prominent near the peripheral capillary dropout. Vascular leakage causes hard exudates which may be peripheral (near the vascular abnormalities) or midperipheral and central (at the macula). In type 1 macular telangiectasia, the telangiectasia and aneurysms with hard exudates (primarily cholesterol) are seen temporal to the fovea. Intraretinal or subretinal fluid/exudates may be noted at the macula.
Exudates vary in size and have a tendency to occupy the inferior pole. As a result, visual acuity is reduced, primarily due to infiltration of the fovea, formation of cystoid macular edema, or even exudative retinal detachment. The exudates ultimately cause discoid glial scarring and subretinal neovascularization; longstanding subretinal exudate may lead to superficial crystalline deposits. The retinal vessels overlying the subretinal exudates may undergo gliotic sheathing. Retinal pigment epithelial metaplasia with subretinal fibrosis may be noted. Retinal neovascularization is uncommon, but can occur in later stages.
The anterior segment is usually not involved in early cases, but neovascularization of the iris or angle of anterior chamber, ectropion uvae, or neovascular glaucoma may be seen in later cases.
In children, the exudative detachment may be bullous, immobile, and touching the posterior capsule of the lens. The irregular caliber of telangiectatic vessels, aneurysms, subretinal exudates, and lack of calcification on ultrasound differentiates Coats disease from retinoblastoma.
Representative cases are presented at https://webeye.ophth.uiowa.edu/eyeforum/cases/100-Coats-Disease.htm and https://webeye.ophth.uiowa.edu/eyeforum/cases/237-Coats-Disease.htm.
Clinical Diagnosis
Besides thorough fundoscopy, which ultimately establishes the diagnosis, several clinical tests may be utilized. Diagnostic tests include OCT, ultrasound, and fluorescence angiography.
Fluorescein angiography
Features of fluorescein angiograms include:
- Telangiectatic vessels
- Aneurysms appearing like light bulbs
- Early and progressive perivascular leakage
- Peripheral capillary nonperfusion
Staging
Staging systems used for Coats disease are listed below.
Gomez-Morales Staging
- Stage I: Focal exudates
- Stage II: Massive exudation
- Stage III: Partial exudative retinal detachment
- Stage IV: Total retinal detachment
- Stage V: Complications
Sigelman Staging
- Stage I: Only telangiactasia
- Stage II: Focal exudates
- Stage III: Partial exudative retinal detachment
- Stage IV: Total retinal detachment
- Stage V: Complications
Shields' classification (usually followed)[3]
- Stage 1: Retinal telangiectasia only
- Stage 2: Telangiectasia and exudation
- A: Extrafoveal exudation
- B.: Foveal exudation
- Stage 3: Exudative retinal detachment
- A: Subtotal detachment
- 1: Extrafoveal
- 2: Foveal
- B: Total retinal detachment
- A: Subtotal detachment
- Stage 4: Total retinal detachment and glaucoma
- Stage 5: Advanced end-stage disease
Differential diagnosis
It is important to differentiate Coats disease from retinoblastoma, since both appear with leukocoria; however, calcium seen on computed tomography or ultrasound is usually a sign of retinoblastoma rather than Coats disease. Other conditions, such as Toxocara infection, retinopathy of prematurity, pars planitis, familial exudative vitreoretinopathy, retinal metastatic lesions, Norrie disease, Eales disease, cavernous retinal hemangioma, and leukemia, may be considered. A retinal vasoproliferative tumor is differentiated by the presence of feeder and draining vessels, an obvious vascular mass, preretinal fibrosis, and extreme peripheral location.
| Feature | Coats Disease | Retinoblastoma |
|---|---|---|
| Presentation | Older patient; unilateral; male | Younger patient; may be bilateral; male and female |
| Leukocoria | Gray to pink | White |
| Telangiectasia | Classic; vessels can be traced | With tumor infiltration; vessels dip into the mass |
| Vitreous seeding | Absent | Maybe present |
| Calcification | Not a feature | Seen on computed tomography and ultrasound |
| Intraocular mass | Not a feature | Seen in endophytic cases |
| Fundus fluorescein angiogram findings | Leaks with telangiectatic vessels | Double circulation |
Management
Treatment
Observation is recommended when the disease involves minimal telangiectatic vessels with little or no exudation and no imminent threat to vision, or in painless and comfortable sightless eyes.
Laser treatment may be given when there is telangiectasia with exudation but no or minimal subretinal fluid. Use at low power for long durations to induce large spot burns to the telangiectatic vessels and aneurysms; peripheral capillary nonperfusion can be given laser treatment, per scatter settings).
Other treatment options include:
- Cryotherapy: For exudation with subretinal fluid of such thickness that the cryotherapy reaction can reach the retina
- Vitreoretinal surgery: For extensive retinal detachment that cannot be treated with laser or cryotherapy
- Enucleation: In cases of painful sightless eyes or when retinoblastoma cannot be ruled out by imaging and clinical examination
- Anti–vascular endothelial growth factor therapy: Has shown promise, but its safety profile in children is still unclear
- Intravitreal triamcinolone acetonide: May reduce the exudation but also increase the risk of glaucoma and cataract
Prognosis
The prognosis depends on the extent of the disease, with milder, older presenting cases, having a better prognosis. In general, children aged <3 years have a poorer prognosis.
Additional Resources
- American Academy of Ophthalmology. 2024–2025 Basic and Clinical Science Course. Section 6: Pediatric Ophthalmology and Strabismus. 2024.
- American Association for Pediatric Ophthalmology and Strabismus. Coats' disease. https://aapos.org/glossary/coats-disease. Accessed April 11, 2025.
- Friedman NJ, Kaiser PK, eds. Case Reviews in Ophthalmology. 2nd ed. Elsevier; 2018.
- Genetic and Rare Diseases Information Center, National Institutes of Health. Coats disease. http://rarediseases.info.nih.gov/gard/6121/coats-disease/. Accessed April 11, 2025.
- Lyons CJ, Lambert SR, eds. Taylor and Hoyt's Pediatric Ophthalmology and Strabismus. 6th ed. Elsevier; 2023.
- Salmon JF, ed. Kanski's Clinical Ophthalmology: A Systematic Approach. 10th ed. Elsevier; 2025.
References
- ↑ Coats G. Forms of retinal diseases with massive exudation. R Lond Ophthalmol Hosp Rep. 1908;17:440-525.
- ↑ 2.0 2.1 Sigler EJ, Randolph JC, Calzada JI, et al. Current management of Coats disease. Surv Ophthalmol. 2014;59(1):30-46.
- ↑ 3.0 3.1 Shields JA, Shields CL, Honavar SG, et al. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001;131(5):572-583.
- ↑ Shields JA, Shields CL, Honavar SG, et al. Clinical variations and complications of Coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001 May;131(5):561-571.